The State of HCP Engagement 2026: Separating Vendor Hype from Commercial Reality
As we approach the 2026 planning cycle, defining the state of HCP engagement has become a challenge of contradictions. On one side, regulatory bodies are tightening the screws on consumer advertising, prompting a scramble for compliant engagement channels. On the other, the “digital transformation” promised since the pandemic has largely plateaued, leaving marketing teams drowning in data but starving for genuine engagement.
A recent wave of vendor-sponsored white papers has begun circulating a common narrative: that Direct-to-Consumer (DTC) is dying, that Healthcare Professionals (HCPs) are begging for higher-frequency email touchpoints, and that Artificial Intelligence (AI) is a plug-and-play solution for personalization.
While these reports capture the anxiety of the market, they often fail to capture the reality of the stakeholder. For commercial leaders (CMOs, VPs of Marketing, and Franchise Heads), accepting these narratives at face value carries significant risk.
By analyzing recent industry findings—including data on regulatory enforcement, HCP preferences, and the shifting workforce—we can construct a more objective roadmap. The goal for 2026 is not “more interaction,” but “precision utility.”
The “Death of DTC” Has Been Greatly Exaggerated
The prevailing industry anxiety was triggered in September 2025, when the FDA launched a “blitz” of warning letters targeting pharmaceutical marketers. The immediate reaction from the vendor ecosystem was predictable: a declaration that the era of DTC is over and that budgets must shift exclusively to HCP engagement.
This is a dangerous overcorrection.
While it is true that Requests for Proposals (RFPs) for 2026 show a marked increase in HCP-focused strategies, the fundamental drivers of DTC remain intact. The regulatory crackdown is focused on specific compliance failures—ambiguity in risk presentation and the misuse of influencers—not on the mechanism of mass-media advertising itself.
The “doom and gloom” narrative ignores the elasticity of the market. Historically, when one channel tightens (e.g., linear TV), spend does not vanish; it migrates to addressable formats like Connected TV (CTV) and programmatic display. The strategic imperative for 2026 is not to abandon the patient journey but to master compliant transparency. The brands that will win are not those that hide risks behind a click, but those that integrate safety data into compelling, “storytelling” creatives that focus on disease state education rather than aggressive brand claims.
The Takeaway: Do not treat HCP marketing as a lifeboat for sinking DTC budgets. Treat them as parallel tracks. If you starve your consumer funnel based on regulatory fear, you risk arriving at the doctor’s office with a brand that patients have never heard of.
The Frequency Fallacy: Why “More” is Not Better
Perhaps the most controversial claim in current vendor literature is that HCPs want more interaction with pharma. Reports suggest that nurse practitioners and physicians prefer communication on a “weekly or biweekly” basis and that the solution to low engagement is simply to increase the cadence of emails and texts.
This “volume-based” view collapses under scrutiny.
We must look at the hard data regarding efficacy. A recent industry study highlighted a staggering disconnect regarding the current state of HCP engagement: while 82% of pharma executives believe their digital outreach is effective, only 28% of HCPs agree. Furthermore, approximately 97% of digital outreach goes completely unanswered.
If 97% of your current volume is ignored, increasing that volume is not a strategy; it is spam.

The issue is not that doctors are “hard to reach”; it is that they are “hard to please” with generic content. The disconnect stems from fragmented data. Most commercial teams still operate with data silos where offline interactions (sales rep visits) are completely disconnected from online behaviors (website clicks). This results in a “blind” bombardment of messages where a doctor might receive a generic “Introduction to [Brand X]” email two days after having a deep-dive clinical discussion with a Medical Science Liaison (MSL).
The Takeaway: The metric for 2026 must shift from Reach to Relevance. Commercial leaders should audit their omnichannel stacks. If your CRM cannot suppress a marketing email based on a rep’s call notes within 24 hours, you are not ready to increase your frequency.
The “New” Gatekeepers: NPs and PAs
If there is one area where the vendor hype aligns with ground truth, it is the demographic shift in prescribing power. The physician-centric model of the past is obsolete.
Employment for Nurse Practitioners (NPs) is projected to grow by 40–45% over the next decade. In many high-volume practices, NPs and Physician Assistants (PAs) have become the primary gatekeepers. Unlike older MDs who may be entrenched in their habits, this cohort is technologically adept; 40% believe AI will enhance outcomes, and they are significantly more open to virtual learning and digital resources than their MD counterparts.
However, marketing to this group requires a tonal shift. Current literature suggests these providers are looking for “educational support” and “financial resource awareness” rather than high-gloss promotional decks. They are often treating underserved populations or managing the day-to-day adherence of chronic patients.
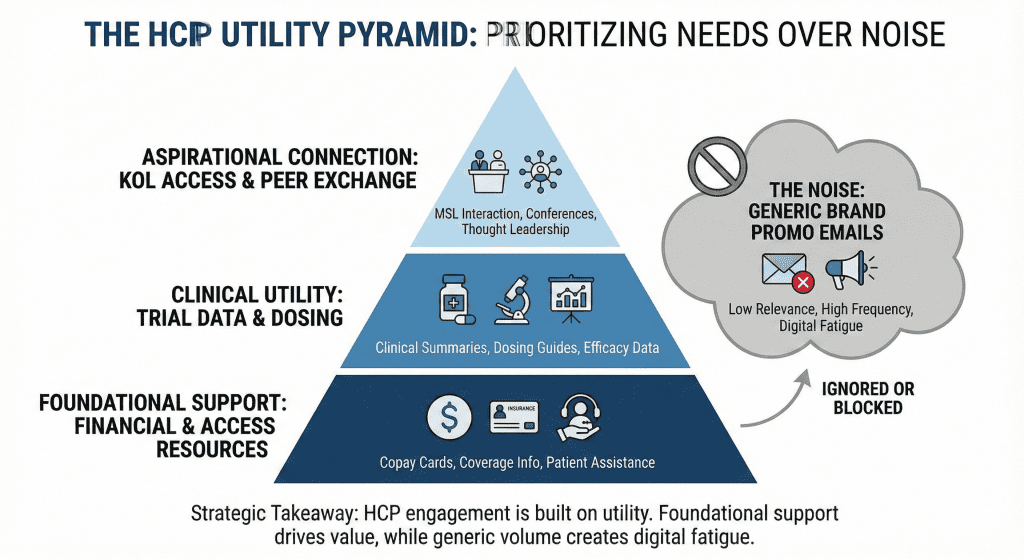
The Takeaway: Your 2026 segmentation strategy is failing if it lumps NPs and PAs into a generic “Allied Health” bucket. They require distinct personas. Content for this group should prioritize patient affordability tools (copay cards, coverage support) and clinical trial summaries, as they are often the ones navigating the logistical hurdles of treatment.
AI: Moving from “Generation” to “Connection”
Artificial Intelligence is the buzzword of the moment, with promises that it will “redefine HCP engagement”. The pitch is seductive: use Generative AI to create thousands of personalized email variations.
However, for leadership, the application of AI should be viewed through a lens of logistics, not just creation.
The most immediate value of AI is not in writing “better” subject lines, but in solving the “last mile” problem of resource connection. HCPs today are overwhelmed by the hunt for information. They do not want a chatty AI bot; they want an AI agent that can instantly retrieve a dosing guide, connect them to a live MSL, or check sample availability without a login barrier.
Furthermore, AI is the only viable solution to the “data silo” problem mentioned earlier. It is the only technology capable of ingesting unstructured data (rep notes, social listening) to build a dynamic profile of the HCP.

The Takeaway: Resist the temptation to use AI solely for content generation (which carries legal/MLR risks). Direct your tech investment toward AI-driven orchestration—tools that predict the next best action for your field force based on digital signals.
Strategic Imperatives for the 2026 Commercial Leader
To navigate the conflicting signals of the market, pharmaceutical leadership should adopt a “Value-Over-Volume” framework.
1. The “Optichannel” Audit
Stop asking “How many emails can we send?” and start asking “How do we stop sending irrelevance?”
Action: Implement “fatigue rules” in your marketing automation platforms. If an HCP has not engaged with three consecutive emails, automatically switch them to a “low-frequency” track focused solely on major clinical updates. This respects their time and preserves your domain reputation.
2. Radical Transparency in DTC
Recognize that the FDA’s scrutiny is a demand for clarity.
Action: Move risk information out of the “fine print” and into the narrative. Use the “Storytelling” approach to focus on the patient condition. This builds trust and insulates the brand from regulatory accusations of minimizing risk.
3. Empower the Mid-Level Practitioner
NPs and PAs are your growth engine, but they are overworked.
Action: Develop “Practice Support Kits” specifically for NPs/PAs. These should not be brand brochures, but utility tools: patient education cheat sheets, unbranded disease state trackers, and one-click access to financial assistance programs.
4. Bridge the Online/Offline Divide
The gap between sales and marketing is costing you credibility.
Action: Integrate your data. A rep should know if a doctor attended a virtual webinar last night. A marketing email should not be sent if a rep is visiting tomorrow. As noted in the industry analysis, “the connection between marketing and sales will no longer be a myth”—but only if leadership mandates shared data infrastructure.
Conclusion
The pharmaceutical sector is not witnessing the “death” of any single channel, nor the magical birth of an AI utopia. We are witnessing a maturation. The days of “spray and pray” marketing—whether on TV or in the inbox—are over, legislated out of existence by the FDA and filtered out of existence by exhausted providers.
Ultimately, the state of HCP engagement in 2026 will be defined by the organizations that respect the intelligence and the time of their customers. They will use data not to target, but to serve. They will use AI not to spam, but to solve. And they will view engagement not as a metric of volume, but as a measure of trust.